M. Carassiti1*, R. Zanzonico1, S. Cecchini2, S. Silvestri2, R. Cataldo1 and F. E. Agrò1
1 Department of Anaesthesia and 2 Research Laboratory of Measurement and Biomedical Instrumentation, University Campus Bio-Medico, Via Álvaro del Portillo, 200, 00128 Rome, Italy
* Corresponding author. E-mail: [email protected]
Background
The forces applied to the soft tissues of the upper airway may have a deleterious effect. This study was designed to evaluate the performance of the GlideScope compared with the Macintosh laryngoscope.
Methods
Twenty anaesthetists and 20 trainees attempted tracheal intubation of a Laerdal SimMan manikin. Forces and pressure distribution applied by both laryngoscope blades onto the soft upper airway tissues were measured using film pressure transducers. The minimal force needed to achieve a successful intubation, in the same simulated scenario, was measured; additionally, we considered the visualization score achieved by using the Cormack–Lehane grades.
Results
All participants applied, on average, lower force with the GlideScope than with the Macintosh in each simulated scenario. Forces [mean (SD)] applied in the normal airway scenario [anaesthetists: Macintosh 39 (22) N and GlideScope 27 (15) N; trainees: Macintosh 45 (24) N and GlideScope 21 (15) N] were lower than forces applied in the difficult airway scenario [anaesthetists: Macintosh 95 (22) N and GlideScope 66 (20) N; trainees: Macintosh 100 (38) N and GlideScope 48 (16) N]. All the intubations using the GlideScope were successful, regardless of the scenario and previous intubation experience. The average pressure on the blades was 0.13 MPa for the Macintosh and 0.07 MPa for the GlideScope, showing a higher uniformity for the latter.
Conclusions
The GlideScope allowed the participants to obtain a successful intubation applying a lower force. A flatter and more uniform pressure distribution, a higher successful rate, and a better glottic view were observed with the GlideScope.
Keywords: forces and pressure distribution; GlideScope laryngoscope; laryngoscopy; Macintosh laryngoscope; manikin
Background
Direct laryngoscopy is the most common procedure performed on the larynx requiring general anaesthesia, and it is a core skill for anaesthetists in the management of the airway. Although direct laryngoscopy is considered the gold standard in tracheal intubation, unexpected difficult intubations are still encountered and failure to secure the airway can drastically increase the morbidity and mortality.1 2 Laryngoscopy can lead to pathological responses of cardiovascular and respiratory systems related to the stimulation of the sympathetic and parasympathetic nervous systems; alterations of haemodynamic parameters, such as heart rate and arterial pressure, and local effects, such as oedema, tooth, and soft tissue lesion, can be caused by excessive forces transmitted through laryngoscope during an intubation.3 4 As a consequence, the reduction in the applied force could drastically reduce the above-mentioned stimulation and the incidence of the other complications.
The attempt to reduce the exerted force and the uncommon, yet critical, failures of direct laryngoscopy to provide an adequate view for tracheal intubation led to the development of alternative devices:5 one of these is the GlideScope videolaryngoscope.6 Increasing evidence indicates that the GlideScope videolaryngoscope has an established role in tracheal intubation,7 decreasing unsuccessful intubation in vitro8 9 and in vivo,10 and the incidence of complications, when compared with the Macintosh laryngoscope.11 12 The main innovation of the videolaryngoscopy consists in the shifting of the point of view in correspondence with the blade’s tip, thanks to a CCD system. The ability to ‘look around the corner’7 allows to change the shape of the blade: while the Macintosh blade has a slight curvature, by which a correct alignment of the three anatomical axes is performed through the application of a high force, the Glide- Scope blade does not require a big effort, as the pronounced curvature angle allows to direct almost immediately the point of view towards the glottis.
Since the ease of obtaining a good view with the use of GlideScope is demonstrated,13 14 the aim of this study is to compare the performances of the two devices when considering, as an objective metric, the minimum effort made by the operator in the attempt to obtain a successful intubation, and the visualization score achieved at this condition, also considering the level of experience of the operator. Although a number of studies have already demonstrated that the applied force is a useful parameter to compare different blades15–19 in direct laryngoscopy, to our knowledge, this is the first study quantifying applied forces with the use of GlideScope.
A considerable scientific effort towards the measurement of force during laryngoscopy17 20–22 for different purposes confirms that the proposed approach could play an important role in the evaluation of laryngoscope performances.
Methods
Forty physicians were recruited to participate in this study. These included 20 consultants (‘anaesthetist’ group) and 20 residents (‘trainee’ group). The anaesthetists had at least 3 yr of experience, and the trainees had at least 1 yr of experience in anaesthesia.
The Macintosh laryngoscope, size 3, and GlideScope videolaryngoscope, middle size, were used in this study.
The participants carried out laryngoscopy on a manikin (SimMan®—Laerdal Airway Management Trainer) using both Macintosh and GlideScope laryngoscopes in a randomized sequence. The airway scenarios were reproduced through the SimMan with the use of its dedicated pneumatic unit: normal airway, tongue oedema, and cervical immobilization.
The minimal pressure and forces, applied by the participants to the soft tissues of the manikin’s upper airways in order to perform a successful intubation, were measured. A failed intubation was defined either as an attempt lasting more than 120 s or as an attempt in which the operator did not intubate even applying the highest force he could: these trials were recorded in order to calculate the rate of success.
During each intubation, the glottis view was scored using the Cormack–Lehane grades:23 CL 1, CL 2, CL 3, and CL 4.
A pressure film transduce
r (LLLW Prescale Pressure Film, Fuji, full scale 0.6 MPa, accuracy 10%) was used to measure the pressure distribution exerted on the blade by the tissues.
The transducer was applied on the tip of the blade in a rectangular region of 240 mm2 (30×8 mm) (Fig. 1).
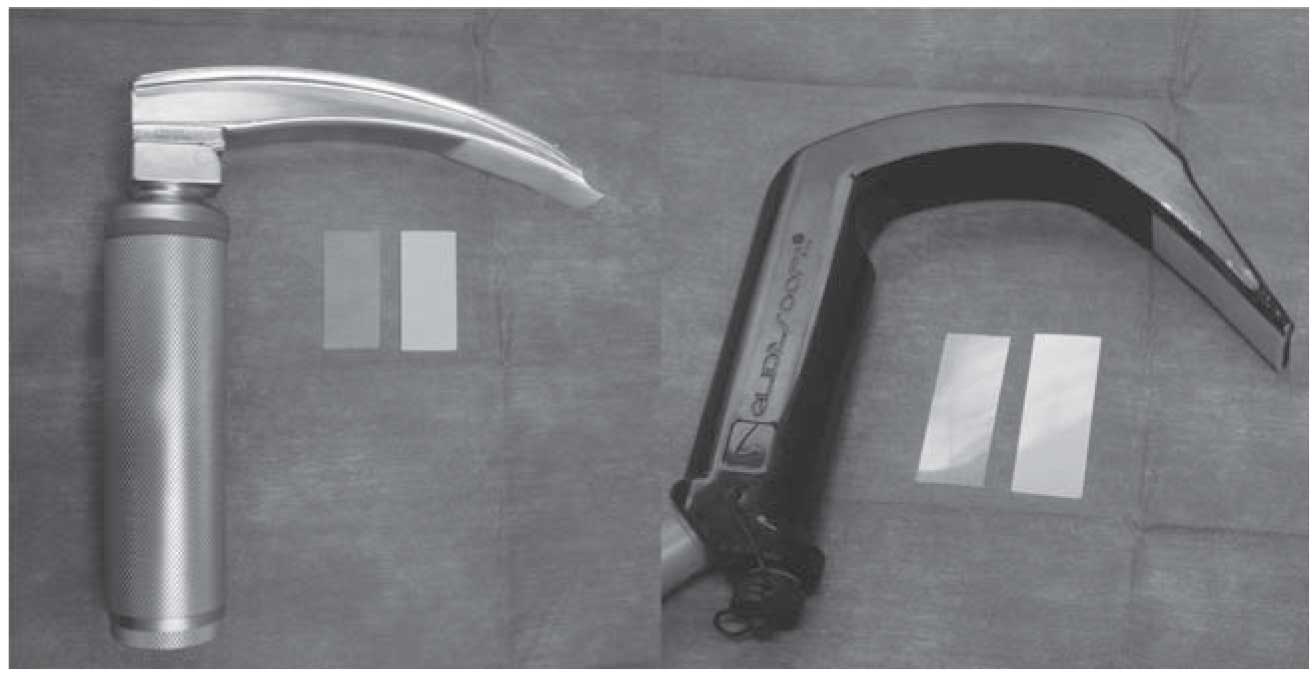
Fig. 1: Positioning of the film transducers on the tips of the laryngoscope blades.
The transducer was composed of two layers. One contained microcapsules full of a colouring fluid substance; the other one was the fixing layer. When the microcapsules broke, the films underwent a colour change proportional to the applied pressure.
After every single intubation, the impressed layer was scanned and processed in order to transform the red optical densities into 256 greyscaled levels. An experimental relation converting the greyscale levels (L: reported in the matrixes) into optical densities (D: reported in ordinates of the graduation curves of the transducer) was obtained by the data provided by the manufacturer (D=10e-0.02L).16 The images were elaborated by a LabVieww-based program, which generated a matrix with the mean greyscale level (red optical density) in every square millimetre of the image. Using the graduation curve of the sensor, it was possible to obtain the pressure intensity with a spatial resolution of 1 mm2. This acquisition and processing chain was first calibrated using coloured samples, provided by the sensor manufacturer, to which known pressure values were associated. The intensity of the resultant force was then calculated by adding the contributions in pressure on each square millimetre of the blade.
Statistical analysis
In order to quantify the dispersion of the measures, all the results are reported as mean (SD).24
A two-tailed t-test was used to assess the dependency of the force applied on the soft tissue on (i) the kind of laryngoscope used during the intubation procedure and (ii) the operator’s level of experience. The test was performed for every airway scenario.
The same test was used to determine whether a significant difference existed between the two devices in the force exerted by the operator at the same Cormack– Lehane score and scenario.
Since multiple scenarios were investigated, repeatedmeasurements analysis of variance (ANOVA) was performed to look for a correlation between the applied force and the difficulty of the airway scenario: normal airway, cervical immobilization, and tongue oedema.
A P-value of ,0.05 was considered statistically significant.
Results
The mean (SD) values of the minimal forces, measured during successful intubations, are shown in Table 1, for every scenario and for both levels of experience. The success rate, representing the number of intubation attempts followed by the tracheal tube positioning above the total, is also reported.
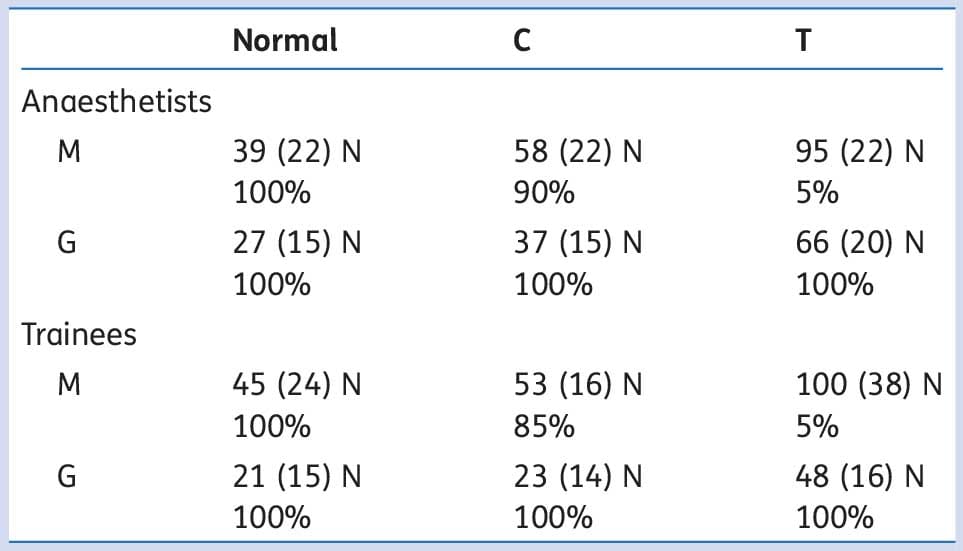
Table 1: Successful rate (%) and forces (N) [mean (SD)] applied by anaesthetists and trainees using either Macintosh (M) or GlideScope (G) in three different scenarios: normal airways (normal), cervical immobilization (C), and tongue oedema (T)
In the anaesthetist group, in the normal airway scenario (Normal), there was not a statistically significant difference between the forces applied with the GlideScope and the Macintosh. In the difficult airway scenarios, both cervical immobilization (C) and tongue oedema (T), the applied force was lower with the GlideScope (P,0.05).
In the trainee group, in all scenarios considered, the applied force was lower with the GlideScope (P,0.05).
Considering the Macintosh laryngoscope, the experience of the operator did not affect the minimal force exerted to succeed in the intubation, while trainees exerted lower force than anaesthetists in the tongue oedema and cervical immobilization scenario when the GlideScope was used (P < 0.05).
With both the Macintosh and the GlideScope, we measured greater applied force with the difficult airways compared with the normal airway (ANOVA: P < 0.05 in each case).
The intubation success rate was inversely related to the difficulty of the airway scenario. With the Macintosh laryngoscope, in the normal airway scenario, all participants obtained a successful tracheal intubation, in the cervical immobilization scenario, 90% of anaesthetists and 85% of trainees could achieve the same result, and in the tongue oedema scenario, only 5% of anaesthetists and 5% of trainees could intubate successfully.
All intubations using the GlideScope were successful, regardless of the scenario and previous intubation experience.
The pressure distribution averaging all participants’ data for the Macintosh and GlideScope blades are shown in Figure 2.
The mean pressure on the blades was 0.13 MPa for the Macintosh and 0.07 MPa for the GlideScope.
In Table 2, the intubations are classified according to the achieved Cormack–Lehane score (CL): the aim is to compare the forces applied with both the devices during intubations, at which equal glottis views were scored.
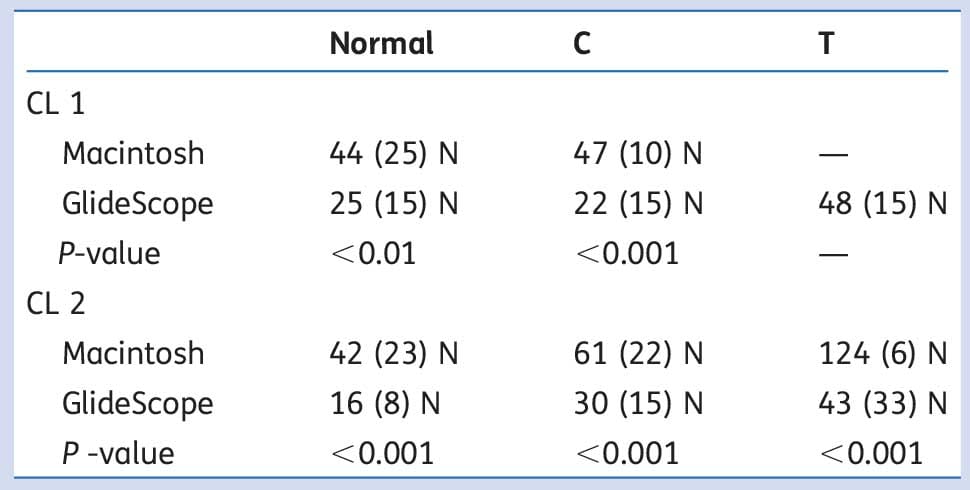
Table 2 Forces [mean (SD)] in the three different scenarios divided considering the glottis view (CL 1 and CL 2): normal airways, cervical immobilization (C), and tongue oedema (T). The P-value indicates the result of a t-test between the two devices
A lower force was exerted with the GlideScope, considering the same glottis view (CL 1 and CL 2) in all scenarios (P < 0.05).
The dashes in Table 2 indicate that no participant was able to achieve a CL 1 with the minimum effort using the Macintosh laryngoscope in the simulated tongue oedema scenario. On the other hand, 12 operators achieved the CL 1 using the GlideScope in the same scenario.
The participants are reported in Table 3 for the visualization score and the device used.
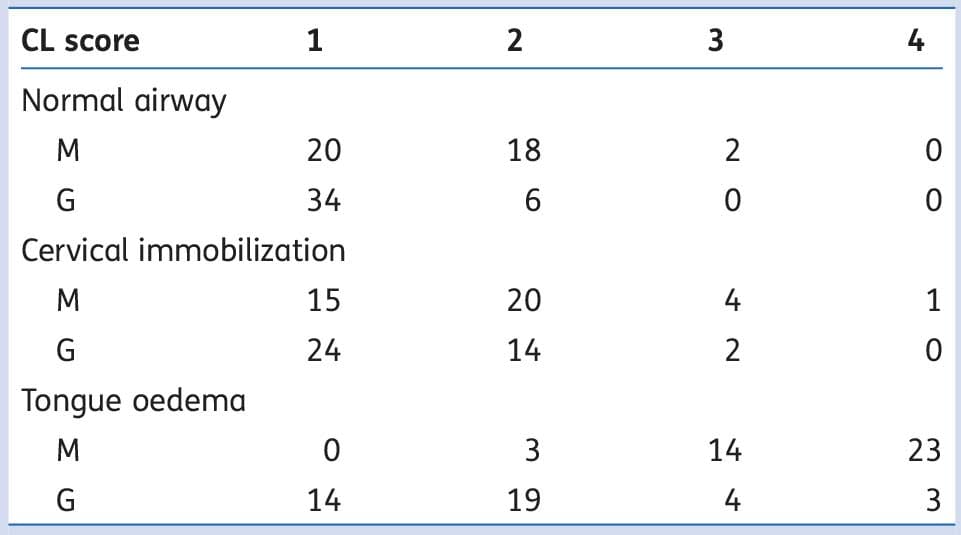
Table 3 Number of participants considering the visualization score and the device used for the intubation: Macintosh (M) and GlideScope (G)
Discussion
Our results show that less effort is needed, less force is applied to the upper airway (Table 1), and flatter and more homogeneous pressure distribution is produced upon the blade (Fig. 2) when a GlideScope is used. Even when the intubation is associated with an equivalent Cormack–Lehane, the minimal applied force required to intubate successfully is lower with the use of the GlideScope for all scenarios considered (Table 2). Moreover, our findings show that with the GlideScope, it is possible to increase the successful intubation rate achieving a better glottic view (Tables 1 and 3), in agreement with the findings by Ahmed-Nusrath,25 where a Cormack–Lehane grade 3 or 4 becomes a grade 1 or 2.
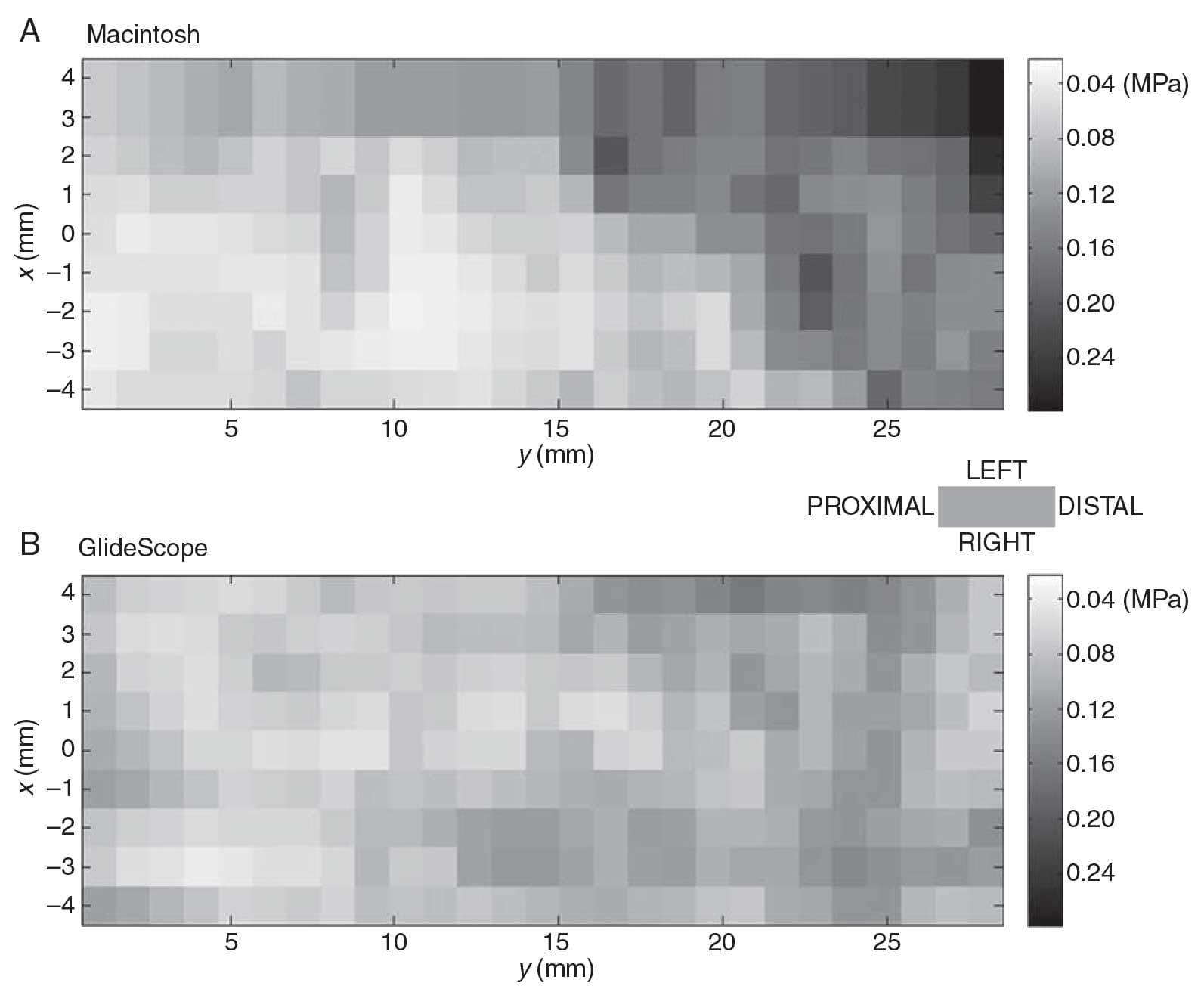
Fig. 2: An example showing pressure distribution on the laryngoscope blades as assessed by using 256 greyscaled levels.
Our results are in accordance with outcomes by Lee and colleagues,15 who demonstrated that video-assisted laryngoscopes seem beneficial when considering applied force as an objective metric of intubation difficulty (in that case, the applied force on maxillary incisors was considered). According to our findings, the force applied by the Anaesthetist group in the normal airway scenario using the Macintosh laryngoscope was 39 (22) N. This is comparable with the 32 (6) N reported under the same conditions (anaesthetists intubating a man
ikin with a Macintosh blade) in our previous study.16 Other surveys present similar results, that is, 38 (2), 33 (13), and 33 (16) N [mean (SD)], respectively, by Hastings and colleagues in vivo,22 and Evans and colleagues,18 and Rassam and colleagues19 on a manikin. Considering the pressure distribution, the Macintosh laryngoscope concentrates the majority of the force on the distal part of the tip, as showed in our previous study.16 Regarding the successful rate, 100%, 97%, and 9% in the normal airway, cervical immobilization, and tongue oedema scenario, respectively, were previously observed when a Macintosh laryngoscope was used.11 In the same study, the overall successful rates with the GlideScope were 100%, 100%, and 89% in the normal airway, cervical immobilization, and tongue oedema scenario, respectively; these results are in line with our outcomes.
In a previous study, it was claimed that the haemodynamic response to intubation might be less with indirect laryngoscopy because of less compression of the soft tissues.26 Our findings further support this statement: we suppose that a lower contact pressure between the soft upper tissues and the laryngoscope blade could also decrease the chance of pharyngeal trauma. Moreover, it is reasonable to assume that a lower applied force allows an easier manoeuvre for operators, in accordance with findings of Malik and colleagues,27 since the procedure requires a lower effort by the operator.
Our method follows a different approach from other studies. Bucx and colleagues20 used a strain gauge-based sensor positioned between the handle and the blade; McCoy and colleagues21 re-designed a laryngoscope handle incorporating a force-displacement transducer; Evans and colleagues18 used a dynamometer; and Hastings and colleagues22 added a metal structure to the handle incorporating two force transducers. The reproducibility of such methods could be limited and the structure of the laryngoscope is somewhat modified in shape and weight, altering the intubation technique.21 Moreover, these devices could be difficult to realize and the measurements difficult to interpret. 20 The study proposed by Santoni and colleagues17 is the first utilizing piezoelectric sensors to measure the applied pressure on six different points of the laryngoscope blade. However, here we increase the resolution of the pressure measurement throughout the surface of the blade by applying pressure sensitive films.
The new-proposed method in this study takes into account two important issues: first, it allowed the procedure to be as spontaneous and natural as possible, without any obstacle to the introductory movement or modification of the device; and second, the measurement set-up was minimally invasive and also easily reproducible in vivo for future purposes.
A limitation must be considered when considering the outcomes of this study. The pressure measurement has been performed on the distal part of the laryngoscope’s blade (30 mm from the tip), neglecting the contributions from the area more proximal to the handle with the hypothesis that the contact with the tongue represented a small percentage of the total. This hypothesis seems to have a valid foundation as our results about forces are in line with findings of previous studies (as regards the Macintosh laryngoscope). 18 19 22 However, as this approximation has been used for both laryngoscopes, considering only the lifting of the glottis would not affect the findings of this survey. Moreover, this is a manikin study and further studies in vivo are needed to strengthen our outcomes.
In conclusion, when compared with the Macintosh laryngoscope, lower forces are applied when the GlideScope is used to achieve tracheal intubation, which may reduce the incidence of side-effects of laryngoscopy, especially in situations of difficult visualization.
Funding
This study was supported by funding from the Department of Anaesthesia at the University Campus Bio-Medico.
References
- Williams KN, Carli F, Cormack RS. Unexpected, difficult laryngoscopy: a prospective survey in routine general surgery. Br J Anaesth 1991; 66: 38–44
- Lai HY, Chen IH, Chen A, Hwang FY, Lee Y. The use of the GlideScopew for tracheal intubation in patients with ankylosing spondilytis. Br J Anaesth 2006; 97: 419–22
- Mort TC. Complications of emergency tracheal intubation: immediate airway-related consequences: Part I. J Intensive Care Med 2007; 22: 157–65
- Mort TC. Complications of emergency tracheal Intubation: immediate airway-related consequences: Part II. J Intensive Care Med 2007; 22: 208–15
- Malik MA, Subramaniam R, Maharaj CH, Harte BH, Laffey JG. Randomized controlled trial of the Pentax AWS®, GlideScope®, and Macintosh laryngoscopes in predicted difficult intubation. Br J Anaesth 2009; 103: 761–8
- Agrò F, Barzoi G, Montecchia F. Tracheal intubation using a Macintosh laryngoscope or a GlideScope in 15 patients with cervical spine immobilization. Br J Anaesth 2003; 90: 705–6
- Sun DA, Warriner CB, Parsons DG, et al. The GlideScope Video Laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth 2005; 94: 381–4
- Ayoub CM, Kanazi GE, Al Alami A, et al. Tracheal intubation following training with the GlideScope compared to direct laryngoscopy. Anaesthesia 2010; 65: 674–8
- Narang AT, Oldeg PF, Medzon R, et al. Comparison of intubation success of video laryngoscopy versus direct laryngoscopy in the difficult airway using high-fidelity simulation. Simul Healthc 2009; 4: 160–5
- Jungbauer A, Schumann M, Brunkhorst V, Bo¨rgers A, Groeben H. Expected difficult tracheal intubation: a prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients. Br J Anaesth 2009; 102: 546–50
- Malik MA, O’Donoghue C, Carney J, et al. Comparison of the Glide- Scope, the Pentax AWS, and the Truview EVO2 with the Macintosh laryngoscope in experienced anaesthetists: a manikin study. Br J Anaesth 2009; 102: 128–34
- Nasim S, Maharaj CH, Malik MA, et al. Comparison of the GlideScope and Pentax AWS laryngoscopes to the Macintosh laryngoscope for use by advanced paramedics in easy and simulated difficult intubation. BMC Emerg Med 2009; 9: 9
- Kaplan MB, Hagberg CA, Ward DS, et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth 2006; 18: 357–62
- Armstrong J, John J, Karsli C. A comparison between the Glide- Scope Video Laryngoscope and direct laryngoscope in paediatric patients with difficult airways—a pilot study. Anaesthesia 2010; 65: 353–7
- Lee RA, Van Zundert AA, Maassen RL, et al. Forces applied to the maxillary incisors during video-assisted intubation. Anesth Analg 2009; 108: 187–91
- Cecchini S, Silvestri S, Carassiti M, Agro` FE. Static forces variation and pressure distribution in laryngoscopy performed by straight and curved blades. Conf Proc IEEE Eng Med Biol Soc 2009; 1: 865–8
- Santoni BG, Hindman BJ, Puttitz CM, et al. Manual-in-line stabilization increases pressures applied by the laryngoscope blade during direct laryngoscopy and orotracheal intubation. Anesthesiology 2009; 110: 24–31
- Evans A, Vaughan RS, Hall JE, et al. A comparison of the forces exerted during laryngoscopy using disposable and nondisposable laryngoscopes blades. Anaesthesia 2003; 58: 869–73
- Rassam S, Wilkes AR, Hall JE, et al. A comparison of 20 laryngoscope blades using an intubating manikin: visual analogue scores and forces exerted during laryngoscopy. Anaesthesia 2005; 60: 384–94
- Bucx MJ, Scheck PA, Van Geel RT, et al. Measurement of forces during laryngoscopy. Anaesthesia 1992; 47: 348–51
- McCoy EP, Mirakhur RK,
Rafferty C, et al. A new device for measuring and recording the forces applied during laryngoscopy. Anaesthesia 1995; 50: 139–43 - Hastings RH, Hon ED, Nghiem C, et al. Force, torque and stress relaxation with direct laryngoscopy. Anesth Analg 1996; 82: 462–8
- Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984; 39: 1105–11
- Joint Committee for Guides in Metrology (JCGM/WG1). Evaluation of measurement data—guide to the expression of uncertainty in measurement. JCGM 2008; 100: 10.
- Ahmed-Nusrath A. Videolaryngoscopy. Curr Anaesth Crit Care 2010; 21: 199–205
- Xue FS, Li XY, Liu QJ, et al. Circulatory responses to nasotracheal intubation: comparison of GlideScope videolaryngoscope and Macintosh direct laryngoscope. Chin Med J (Engl) 2008; 121: 1290–6
- Malik MA, Hassett P, Carney J, et al. A comparison of the Glide- Scope, Pentax AWS, and Macintosh laryngoscopes when used by novice personnel: a manikin study. Can J Anesth 2009; 56: 802–11


