TOSHIAKI TAKAHASHI, YUKIHISA WADA, HIROSHI YAMAMOTO
From Kochi Medical School, Kochi, Japan
We measured the pressure distribution across the tibiofemoral and patellofemoral joints during total knee arthroplasty (TKA) using Fuji pressure-sensitive film (Prescale) in 51 patients (63 joints) comparing the results with those in 21 patients in whom Prescale was not used.
We classified the stress-distribution patterns in the tibiofemoral joints into four types: normal, varus-valgus instability, rotational malalignment, and a combination of instability and malrotation. The medial ligaments were then released according to the information obtained from these patterns. The conformity ratio of the contact area between repeated trials was 87.0%. Pressure distribution across the patellofemoral joints was also considered.
There was a significant decrease in the mean valgus stress angle in the Prescale group compared with the control group (p < 0.01). Release of the lateral retinaculum according to the results showed no significant differences in subluxation of the patella between the released group and the group which did not appear to need this procedure.
Instability of the tibiofemoral and patellofemoral joints is a common cause of dysfunction after total knee arthroplasty (TKA).1,2 It may occur because of ligamentous imbalance, improper design of the prosthesis or inadequate positioning of the components.3 Adequate release of the medial ligaments and lateral retinaculum is important to obtain a stable knee with good congruence in both joints. Contact forces which are not balanced during load-bearing and active movement may lead to loosening of the prosthesis and increased wear of the polyethylene.4 We measured the stress distribution at the surfaces of the tibiofemoral and patellofemoral joints during operation for TKA using Fuji pressure-sensitive film (Prescale; Fuji Photo Film Co Ltd, Japan) to determine whether this may help to assess the need for soft-tissue release.
PATIENTS AND METHODS
Since 1990, we have measured the pressure distribution during TKA in 63 joints in 51 patients. There were seven men and 44 women; 43 had osteoarthritis and 8 rheumatoid disease. Their mean age was 71 years (50 to 85). Another 21 patients (28 joints) were operated on without using Prescale film and were used as a control group; of these 18 had osteoarthritis and 3 had rheumatoid arthritis. Their mean age was 68 years (55 to 82). All patients were operated on by the same surgeon and received an MG-type TKA (Zimmer Inc). There was no significant difference between the two groups in age, gender, or diagnosis.
Prescale film consists of two thin sheets, between which lies a layer of microcapsules. The higher the pressure is the greater the number of microcapsules which rupture, creating a stronger image. The unit area of measurement has a resolution of 0.1 mm.2 We used low-pressure Prescale film which registers pressure between 2.5 and 10 MPa; this was used in a waterproof package and sterilised with ethylene oxide gas. The thickness of the film is 0.4 mm including the laminate. To fit the surface of the tibiofemoral joint, the material was prepared in three sizes. For the patellofemoral joint, nearly elliptical shapes with wings for pin fixation were used.
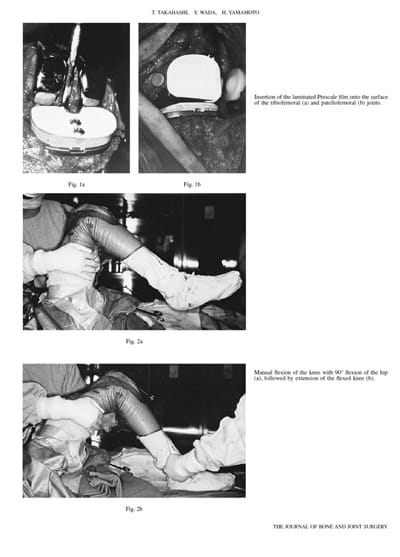
Figure 1 shows the insertion of the Prescale film. For the tibiofemoral joint it was fixed with screws to the trial tibial component to prevent any movement on the joint surface
(Fig. 1a). For the patellofemoral joint, the reduced patella was stabilised by clamping its medial border to the incised quadriceps expansion using three towel clips.
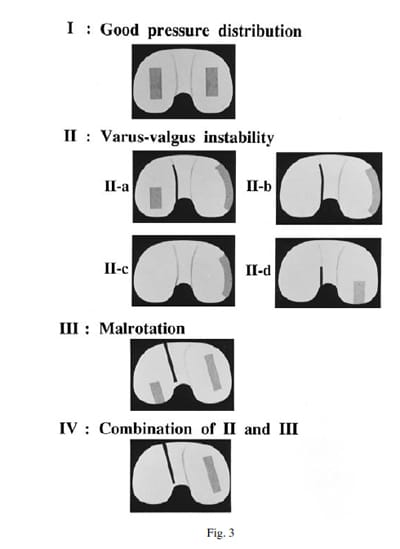
For each test the knee was flexed once only by manual flexion of the hip while holding only the thigh, with no abduction or adduction of the hip (Fig. 2a). This allowed flexion of the knee to 90° produced by the weight of the lower leg. The joint was then extended smoothly, using one finger behind tendo Achillis (Fig. 2b). The Prescale film was removed from the tibiofemoral joint and a similar procedure followed for the patellofemoral joint (Fig. 1b). The contact areas as determined by the stained film were then examined.
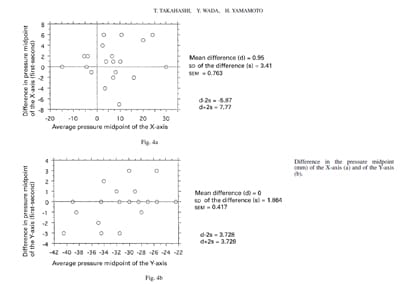
We classified the stress distribution in the tibiofemoral joints into four patterns (Fig. 3). Pattern I showed uniform bilateral contact – no release of the medial collateral ligament was performed. Patterns IIa, IIb, and IIc were seen in mild, moderate and severe varus-valgus instability respectively, with increased loading concentrated at the inner margin of the compartment on the convex side. In pattern IIa, loading was also observed at the centre of the other side (the lateral compartment in a varus knee). In pattern IIb, the maximal loading had moved to the inner margin of this compartment and in IIc loading was confined to the compartment on the convex side. When pattern II was seen, the medial collateral ligament was released near the level of the joint surface. If pattern II was still present when Prescale film was used again, subperiosteal stripping of the pes anserinus from the proximal tibia was added. If this did not correct the appearance to pattern I the posteromedial capsule was also released. For pattern IIa, release of the medial collateral ligament alone was always sufficient, but release of the pes anserinus or stripping of the posteromedial capsule was often required for patterns IIb and IIc. In pattern IId, stress was concentrated in the posterior region of the medial compartment, and release of the posteromedial capsule was always required. Pattern III was produced by rotational malalignment and required adjustment of the tibial component. Pattern IV was seen when there was a combination of varus-valgus instability and malrotation; this indicated the need for a combination of the procedures carried out for patterns II and III.
We classified the patellofemoral contact patterns into three types: type A had a normal loading on both medial and lateral facets; type B showed reduced loading; and type C absence of loading on the medial side. Pattern A did not require release of the lateral retinaculum. For pattern type B, release was performed only at the level of the patella and for type C from the level of the tibial tuberosity to the superior margin of the patella. On retesting, if stress distribution was still unbalanced the release was extended proximally along the lateral border of t
he vastus lateralis. Adequate release of the lateral retinaculum allowed equal contact on both sides of the patella. We studied the reproducibility of the pressure distribution in the tibiofemoral joint, by repeating the test twice under the same conditions in 20 joints. An analyser (Fuji film Pressuregraph FPD-703) was used to measure the pressure of the contact area (over 2.5 MPa), the mean and maximal contact pressure, and the midpoint of the pressure distribution.
Instability of the tibiofemoral joint was assessed after TKA by obtaining stress radiographs with forces of 150 N laterally and medially to the knee in nearly full extension, using a Telos stress divice. The lateral shift and tilt of the patella were evaluated on axial films after operation. We compared the postoperative range of movement and the radiological findings for varus and valgus stress between the Prescale and control groups. We analysed the usefulness of measuring the tibiofemoral and patellofemoral contact using a two-sample t-test, and the reproducibility of our methods by linear regression analysis.
RESULTS
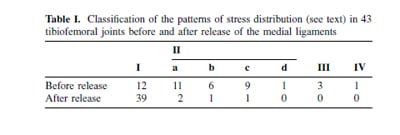
In order to analyse the reproducibility of repeated trials the midpoint of the pressure distribution was determined by defining the coronal plane (medial/lateral) as the X-axis and the sagittal plane (anterior/posterior) as the Y-axis (Figs 4a and 4b). In a series of 20 measurements the limits of
agreement (d-2s to d+2s) were small enough for us to be confident that the midpoint of the pressure distribution as measured with the Pressuregraph analyser was within reasonable limits for our method.
Of the 43 joints in which the stress distribution was examined before and after release of the medial ligaments, 12 (28%) showed good stress distribution which did not require release of the medial ligament. The most common pattern showed a varus-valgus instability in 27 joints (63%). Malrotation requiring correction of the tibial component was found in three joints (7%), and one showed a combination of varus-valgus and rotational malalignment (Table I). After completion of releases a good distribution of loading stress was observed in 39 joints (91%), but a varus-valgus instability pattern was still present in four.
Of the 49 patellofemoral joints examined, 21 (43%) were type A with equal pressures, 12 (24%) were type B, and 16 (33%) were type C with lateral pressure only. The mean preoperative and postoperative lateral shift of the patella was 4.9 mm and 4.8 mm respectively in the group without release (type A) and 4.8 mm and 2.4 mm respectively in those with release (types B and C). The mean tilting of the patella before and after the operation was 5.1° and 2.3° respectively in the group without release and 4.4° and 1.1° respectively in those undergoing release. There was no significant difference between the two groups in lateral shift or tilting (p > 0.05). Dislocation of the patella did not occur.
The mean range of knee movement was 97° before and 106° after operation in the Prescale group (p < 0.05). In the control group the range was 110° before and 112° after operation, showing no significant difference.
The mean valgus stress angle as a measure of varusvalgus instability of the tibiofemoral joint was 4.0° in the Prescale group and significantly more (5.6°) in the control group (p < 0.01). There was no significant difference in the mean varus stress angle between the two groups. The mean valgus plus varus stress angle was 9.2° in the Prescale group and 11.6° in the control group (p < 0.02).
DISCUSSION
In deformed arthritic knees, contractures of the ligaments and articular capsule may require progressive release of the medial collateral ligaments, pes anserinus, and postero medial capsule during TKA. This is difficult to judge5 and excessive release may lead to joint instability and failure of the operation. Careful attention is needed to obtain a proper ligamentous balance. Wasielewski et al6 confirmed that the adequacy of ligament release during operation is closely related to the pattern and severity of polyethylene wear as found at revision.
Measurement of the tone of the ligaments7 and of the pressure at the articular surface is useful in assessing the proper release of soft tissues at the tibiofemoral joint. Our method of analysis of contact pressure is applied at the correct anatomical sites and can also evaluate malrotation.
There have been several reports on the evaluation of contact areas and stress distribution in artificial knees.8-11 These studies, however, were performed on cadavers or with components alone, and did not address the value of measurements during operation as a guide to the release of soft tissues or the positioning of the components.
In the patellofemoral joint, correction of tracking abnormalities are important to allow proper congruence. Release of the lateral retinaculum and even shortening of the medial retinaculum are performed but the lateral release may damage branches of the lateral genicular artery. For this reason its use should be limited to cases of definite subluxation. 12 Judgement of the need for such procedures is difficult; assessment of pressures in the patellofemoral joint may be useful. We found that 43% of our patients did not require lateral release, since the intraoperative evaluation of the pressure distribution showed adequate congruency without this operation.
After operation, lateral stability at the tibiofemoral joint was better in the Prescale group than in the control group because release was used less often, but there was no difference in the range of movement. Harvey et al13 also reported that the postoperative range of movement was not influenced significantly by medial release of the collateral ligament. Extended release does not increase range of movement, and may prejudice the stability of the joint.
One disadvantage of our method is that measurements are made during passive and not active movements; adequate quadriceps tension may not have been applied.
We attempted to reproduce the contact stress during walking by the manual application of intraoperative axial loading. The patterns for the tibiofemoral joint were similar to those obtained by passive knee movement, but it was difficult to apply the load at constant force and direction.
In our study, medial ligament release was performed only after the analysis of contact patterns, and after operation we consistently obtained varus-valgus stability. We consider that the intraoperative measurement of contact forces is a useful means of detecting imbalance at the tibiofemoral joint and in assessing patellar tracking.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
REFERENCES
- Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop 1988;226:49-64.
- Fehring TK, Valadie AL. Knee instability after total knee arthroplasty. Clin Orthop 1994;299:157-62.
- Tew M, Waugh W. Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg [Br] 1985;67-B:551-6.
- Hsu HP, Garg A, Walker PS, Spector M, Ewald FC. Effect of knee component alignment on tibial load distribution with clinical cor
relation. Clin Orthop 1989;248:135-44. - Sambatakakis A, Wilton TJ, Newton G. Radiographic sign of persistent soft-tissue imbalance after knee replacement. J Bone Joint Surg [Br] 1991;73-B:751-6.
- Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop 1994;299:31-43.
- Shoji H, Yoshino S, Komagamine M. Improved range of motion with the Y/S total knee arthroplasty system. Clin Orthop 1987;218:150-63.
- Walker PS, Hsu H-P, Zimmerman RA. A comparative study of uncemented tibial components. J Arthroplasty 1990;5:245-53.
- Buechel FF, Pappas MJ, Makris G. Evaluation of contact stress in metal-backed patellar replacements: a predictor of survivorship. Clin Orthop 1991;273:190-7.
- McNamara JL, Collier JP, Mayor MB, Jensen RE. A comparison of contact pressures in tibial and patellar total knee components before and after service in vivo. Clin Orthop 1994;299:104-13.
- Szivek JA, Cutignola L, Volz RG. Tibiofemoral contact stress and stress distribution evaluation of total knee arthroplasties. J Arthroplasty 1995;10:480-91.
- Ranawat CS. The patellofemoral joint in total condylar knee arthroplasty: pros and cons based on five- to ten-year follow-up observations. Clin Orthop 1986;205:93-9.
- Harvey IA, Barry K, Kirby SPJ, Johnson R, Elloy MA. Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg [Br] 1993;75-B:950-5.